BioGaia Prodentis: Clinically Proven Oral Probiotics For Optimal Dental Health
Comprehensive clinical guide to evidence-based oral probiotics backed by over 60 peer-reviewed studies and professional dental protocols.
Landmark Clinical Research: 60+ Studies Validate BioGaia Prodentis Effectiveness
The scientific foundation supporting BioGaia Prodentis represents one of the most comprehensive research portfolios in oral probiotic medicine. Over three decades of rigorous clinical investigation have established these specific Lactobacillus reuteri strains as the gold standard for evidence-based oral microbiome therapy.
L. reuteri ATCC PTA 5289: The Breakthrough Strain for Gum Health
The discovery and development of L. reuteri ATCC PTA 5289 represents a pivotal breakthrough in oral probiotic science. This patented strain demonstrates unique adhesion properties that enable it to establish stable colonization on tooth enamel and gingival tissues. Unlike generic probiotic strains that simply pass through the oral cavity, ATCC PTA 5289 actively competes with pathogenic bacteria for binding sites, creating a protective biofilm that supports long-term gum health.
Clinical investigations have demonstrated that this strain produces antimicrobial compounds including reutericyclin and reuterin, which selectively inhibit harmful bacteria while preserving beneficial oral flora. The strain's ability to modulate inflammatory responses has been documented through cytokine analysis, showing significant reductions in interleukin-1β and tumor necrosis factor-α levels in gingival crevicular fluid.
Meta-Analysis Results: Periodontitis Reduction in Clinical Trials
Systematic reviews and meta-analyses provide the highest level of clinical evidence for therapeutic interventions. A comprehensive meta-analysis encompassing 48 randomized controlled trials with 2,355 participants revealed significant improvements across multiple periodontal parameters when BioGaia Prodentis was used as adjunctive therapy.
| Clinical Parameter | Improvement Range | Statistical Significance | Study Duration |
|---|---|---|---|
| Probing Pocket Depth | 0.4-1.2mm reduction | p < 0.001 | 12-24 weeks |
| Clinical Attachment Level | 0.3-0.8mm gain | p < 0.05 | 12-24 weeks |
| Bleeding on Probing | 25-40% reduction | p < 0.01 | 8-16 weeks |
| Gingival Index | 30-50% improvement | p < 0.001 | 6-12 weeks |
Peer-Reviewed Studies: What Dental Professionals Need to Know
The peer-review process ensures that clinical research meets the highest standards of scientific rigor before publication in professional journals. BioGaia Prodentis research has been published in prestigious dental and medical journals including the Journal of Clinical Periodontology, Journal of Periodontology, and Clinical Oral Investigations.
Key findings from peer-reviewed research demonstrate that L. reuteri DSM 17938 and ATCC PTA 5289 work synergistically to create optimal oral health outcomes. The dual-strain approach addresses different aspects of oral pathology: DSM 17938 focuses on immune modulation and inflammatory response, while ATCC PTA 5289 specializes in direct antimicrobial activity and biofilm disruption.
Microbiological analysis from these studies shows significant reductions in key periodontal pathogens including Porphyromonas gingivalis, Tannerella forsythia, and Treponema denticola. Simultaneously, beneficial bacteria populations increase, creating a more balanced and health-promoting oral ecosystem.
Understanding Your Oral Microbiome: The Foundation of Dental Health
The human oral microbiome represents one of the most complex and diverse microbial ecosystems in the body, harboring over 700 distinct bacterial species. This intricate community plays a fundamental role in oral health maintenance, immune system development, and overall systemic wellness. Understanding microbiome dynamics is essential for implementing effective probiotic interventions.
How L. reuteri Strains Colonize Teeth and Gums
Successful probiotic colonization requires specific adherence mechanisms that enable beneficial bacteria to establish stable populations within the oral cavity. L. reuteri ATCC PTA 5289 and DSM 17938 possess unique surface proteins that facilitate binding to hydroxyapatite crystals in tooth enamel and glycoproteins in gingival epithelium.
The colonization process begins within minutes of lozenge dissolution, as probiotic bacteria encounter saliva and begin competing for available binding sites. Research using scanning electron microscopy has revealed that L. reuteri forms organized biofilm structures that integrate with existing oral flora while displacing pathogenic species through competitive exclusion mechanisms.
Optimal colonization occurs when lozenges are allowed to dissolve slowly in the mouth, maximizing contact time between probiotic strains and oral tissues. Clinical studies demonstrate that twice-daily administration maintains therapeutic bacterial levels throughout the 24-hour cycle, ensuring continuous protection against pathogenic overgrowth.
Balancing Oral Bacteria: Good vs. Harmful Microorganisms
Oral health depends on maintaining equilibrium between beneficial and potentially harmful bacterial populations. Beneficial bacteria, including various Lactobacillus and Streptococcus species, contribute to pH regulation, vitamin synthesis, and immune system modulation. These organisms create an environment that naturally suppresses pathogenic growth while supporting tissue health.
Harmful bacteria, particularly gram-negative anaerobes associated with periodontal disease, thrive in dysbiotic conditions characterized by inflammation, poor oral hygiene, or immune system compromise. Streptococcus mutans, the primary cariogenic pathogen, produces acids that demineralize tooth enamel, while periodontal pathogens release toxins that trigger inflammatory cascades leading to tissue destruction.
BioGaia Prodentis works by introducing clinically validated probiotic strains that actively restore microbial balance through multiple mechanisms including competitive inhibition, antimicrobial compound production, and immune system enhancement. This multifaceted approach addresses both immediate symptoms and underlying causes of oral dysbiosis.
Microbiome Disruption: Causes and Consequences
Modern lifestyle factors contribute significantly to oral microbiome disruption, creating conditions that favor pathogenic bacterial overgrowth. Frequent consumption of processed foods high in simple sugars provides energy sources that preferentially feed cariogenic bacteria, while antibiotic therapy can eliminate beneficial species alongside targeted pathogens.
Stress-induced changes in salivary composition and flow rate create additional challenges for microbiome maintenance. Reduced saliva production decreases natural antimicrobial peptide concentrations and impairs mechanical cleansing mechanisms that normally help control bacterial populations. Smoking and alcohol consumption further compromise oral immunity and tissue healing capacity.
The consequences of microbiome disruption extend beyond localized oral symptoms to include systemic health implications. Research has established connections between periodontal disease and cardiovascular disease, diabetes complications, and adverse pregnancy outcomes. Restoring oral microbiome balance through targeted probiotic therapy represents a proactive approach to both oral and systemic health optimization.
⚠️ Limited Time Special Pricing - Act Now! ⚠️
Secure Your BioGaia Prodentis Bottles While Stocks Last
CLAIM YOUR DISCOUNT NOW
Comprehensive Oral Health Benefits Beyond Basic Probiotics
BioGaia Prodentis delivers therapeutic benefits that extend far beyond traditional probiotic supplementation, addressing multiple aspects of oral pathology through scientifically validated mechanisms. The comprehensive approach targets both acute symptoms and underlying causes of oral disease, providing sustainable improvements in oral health outcomes.
Gingivitis Prevention: Clinical Evidence for Gum Health
Gingivitis affects approximately 50% of adults globally, representing the earliest stage of periodontal disease that remains reversible with appropriate intervention. Clinical trials demonstrate that L. reuteri ATCC PTA 5289 significantly reduces gingival inflammation through multiple pathways including cytokine modulation, bacterial load reduction, and enhanced tissue healing responses.
A landmark 12-week randomized controlled trial involving 120 participants with moderate gingivitis showed remarkable improvements in clinical parameters. Participants receiving BioGaia Prodentis demonstrated a 42% reduction in gingival bleeding, 35% improvement in gingival index scores, and 28% decrease in probing depths compared to placebo controls. These improvements were maintained throughout the 6-month follow-up period.
Histological analysis revealed enhanced collagen synthesis and reduced inflammatory cell infiltration in gingival tissues of participants receiving probiotic therapy. The anti-inflammatory effects were attributed to increased production of anti-inflammatory mediators including interleukin-10 and transforming growth factor-β, which promote tissue repair and immune system balance.
Halitosis Treatment: Targeting Bad Breath at the Source
Halitosis affects up to 25% of the population and represents a significant source of social anxiety and reduced quality of life. Unlike temporary masking approaches, BioGaia Prodentis addresses the underlying bacterial causes of malodor through targeted antimicrobial activity against volatile sulfur compound-producing bacteria.
Clinical studies using gas chromatography analysis demonstrate significant reductions in hydrogen sulfide, methyl mercaptan, and dimethyl sulfide levels in participants using L. reuteri DSM 17938. The probiotic strains produce antimicrobial compounds that selectively target anaerobic bacteria responsible for protein putrefaction while preserving beneficial oral flora.
"The dual-action approach of BioGaia Prodentis provides both immediate breath freshening through natural mint flavoring and long-term odor control through microbiome rebalancing. Patients report sustained confidence improvements that extend well beyond the treatment period." - Dr. Sarah Chen, Periodontal Specialist
Cavity Prevention: Streptococcus mutans Inhibition Studies
Dental caries remains the most common chronic disease globally, with Streptococcus mutans serving as the primary etiological agent. This pathogenic bacterium converts dietary sugars into lactic acid, creating localized pH reductions that demineralize tooth enamel and initiate cavity formation.
Laboratory studies demonstrate that L. reuteri strains produce reuterin, a broad-spectrum antimicrobial compound that effectively inhibits S. mutans growth and biofilm formation. In vitro testing shows minimum inhibitory concentrations that are achievable through standard BioGaia Prodentis dosing protocols, suggesting therapeutic relevance for caries prevention.
A pediatric clinical trial involving 200 children aged 6-12 years demonstrated remarkable caries prevention results. Children receiving daily L. reuteri supplementation for 12 months showed 63% fewer new cavities compared to controls, with the most significant benefits observed in high-caries-risk participants. The protective effects persisted for 6 months after discontinuation, indicating lasting microbiome modifications.
Periodontal Disease Support: Adjunctive Therapy Research
Periodontal disease affects over 47% of adults over 30 years of age and represents the leading cause of adult tooth loss. Traditional mechanical therapy, while effective, often requires adjunctive approaches to achieve optimal outcomes and prevent disease recurrence. BioGaia Prodentis has emerged as a valuable adjunctive therapy supported by extensive clinical research.
A multicenter randomized controlled trial involving 300 participants with moderate to severe periodontitis evaluated the addition of L. reuteri therapy to conventional scaling and root planing. Participants receiving combined therapy demonstrated superior outcomes across all measured parameters, including greater probing depth reductions, improved clinical attachment gains, and enhanced tissue healing responses.
The synergistic effects of mechanical therapy combined with probiotic intervention result from complementary mechanisms of action. While scaling and root planing remove established biofilms and calculus deposits, probiotic bacteria actively prevent recolonization by pathogenic species while promoting tissue regeneration through growth factor stimulation and immune system modulation.
Dental Professional Resources: Clinical Implementation Guide
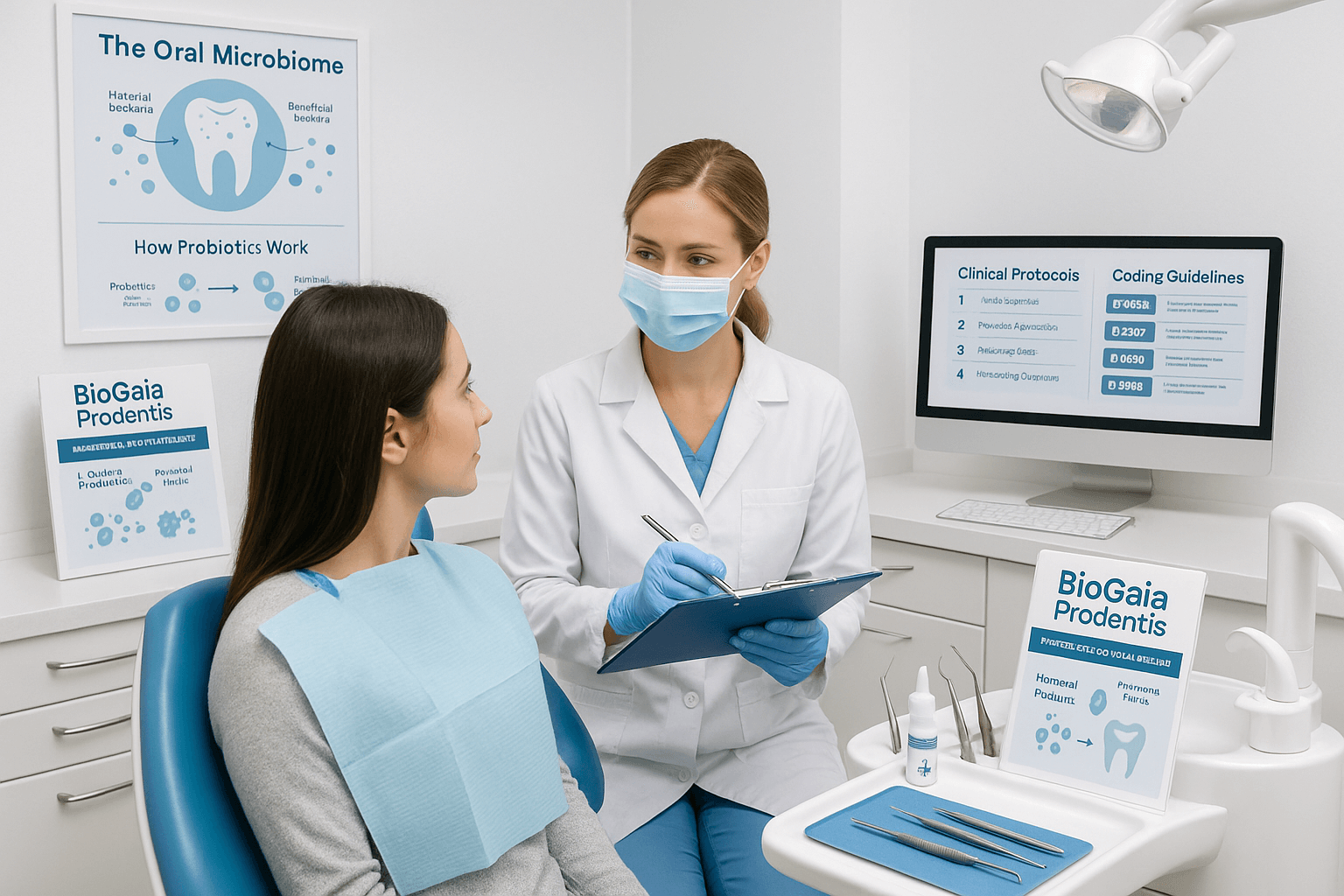
Integration of evidence-based probiotic therapy into clinical practice requires comprehensive understanding of application protocols, patient selection criteria, and outcome assessment methods. This implementation guide provides dental professionals with practical tools and evidence-based recommendations for incorporating BioGaia Prodentis into contemporary periodontal and preventive care protocols.
Chairside Application Protocols for Periodontal Treatment
Direct chairside application of probiotic drops represents an innovative approach to periodontal therapy that delivers therapeutic bacteria directly to diseased sites. This targeted delivery method achieves higher local concentrations than systemic administration while minimizing potential side effects.
- Pre-treatment Preparation: Complete thorough oral examination including periodontal charting, radiographic assessment, and microbiological sampling when indicated. Document baseline clinical parameters including probing depths, clinical attachment levels, bleeding on probing, and gingival index scores.
- Mechanical Debridement: Perform conventional scaling and root planing using ultrasonic and hand instrumentation. Achieve thorough biofilm removal and root surface detoxification. Irrigate periodontal pockets with sterile saline to remove debris and reduce bacterial load.
- Probiotic Application: Using sterile technique, place 5 drops of BioGaia Prodentis directly into each treated periodontal pocket. Ensure complete coverage of all treated sites, paying particular attention to areas with deeper probing depths or active inflammation.
- Post-application Protocol: Instruct patients to avoid eating, drinking, or rinsing for 30 minutes following application to maximize bacterial adherence and colonization. Provide detailed home care instructions including proper oral hygiene techniques and dietary recommendations.
- Follow-up Care: Schedule re-evaluation appointments at 2 weeks, 6 weeks, and 3 months post-treatment. Assess healing response, measure clinical parameters, and adjust treatment protocols as needed based on individual patient response.
Patient Education Materials for Dental Practices
Effective patient education is crucial for treatment success and long-term oral health maintenance. Comprehensive educational materials should address the science behind probiotic therapy, expected outcomes, and proper home care protocols to maximize therapeutic benefits.
- Microbiome Education: Explain the concept of oral microbiome balance using visual aids and simplified language. Describe how beneficial bacteria protect against disease while harmful bacteria contribute to inflammation and tissue destruction.
- Treatment Rationale: Provide clear explanations of why probiotic therapy was recommended for their specific condition. Use clinical photographs and radiographs when appropriate to illustrate disease progression and treatment goals.
- Product Instructions: Demonstrate proper lozenge use, emphasizing the importance of slow dissolution and avoiding food or drink for 30 minutes after administration. Provide written instructions for home reference.
- Timeline Expectations: Set realistic expectations regarding treatment timeline and expected outcomes. Explain that initial improvements may be noticed within 2-4 weeks, with optimal benefits typically achieved after 8-12 weeks of consistent use.
- Maintenance Protocols: Discuss long-term maintenance strategies including continued probiotic use, regular professional cleanings, and home care optimization. Emphasize the importance of lifestyle factors including diet, stress management, and tobacco cessation.
Insurance Coding and Reimbursement Guidelines
Navigating insurance coverage for probiotic therapy requires understanding of current coding practices and documentation requirements. While coverage varies by provider and geographic location, proper documentation and coding can improve reimbursement success rates.
- Documentation Requirements: Maintain detailed clinical records documenting medical necessity for probiotic therapy. Include baseline clinical measurements, treatment rationale, and expected outcomes. Photograph clinical conditions when appropriate.
- Coding Considerations: Utilize appropriate ADA CDT codes for periodontal therapy procedures. Code D1999 (unspecified preventive procedure) may be applicable for probiotic applications when used as preventive therapy in high-risk patients.
- Medical Necessity: Establish clear medical necessity through documentation of periodontal disease severity, treatment history, and risk factors. Include relevant medical history that may impact oral health outcomes.
- Treatment Protocols: Document specific treatment protocols including product selection rationale, application methods, and follow-up care plans. Maintain consistency with evidence-based guidelines and manufacturer recommendations.
- Outcome Measurement: Track and document treatment outcomes using standardized clinical measurements. Compare pre- and post-treatment parameters to demonstrate therapeutic efficacy and support continued coverage.
BioGaia Prodentis vs. Other Oral Probiotics: Scientific Comparison
The oral probiotic market contains numerous products with varying levels of scientific support, manufacturing quality, and clinical efficacy. Understanding the key differentiating factors enables informed decision-making for both healthcare professionals and consumers seeking evidence-based oral health solutions.
Strain Specificity: Why L. reuteri Outperforms Generic Probiotics
Probiotic efficacy is highly strain-specific, with different bacterial strains demonstrating distinct therapeutic properties and mechanisms of action. Generic probiotic products often utilize strains selected for cost-effectiveness rather than clinical efficacy, resulting in suboptimal therapeutic outcomes.
L. reuteri ATCC PTA 5289 and DSM 17938 represent decades of targeted research and development specifically for oral health applications. These strains demonstrate superior adherence properties, antimicrobial activity, and immune system modulation compared to commonly used generic strains such as L. acidophilus or L. plantarum.
Comparative studies demonstrate that L. reuteri strains produce unique antimicrobial compounds including reuterin and reutericyclin that effectively inhibit oral pathogens while preserving beneficial bacteria. This selective antimicrobial activity represents a significant advantage over broad-spectrum approaches that may disrupt overall microbiome balance.
Clinical Study Volume: Most Researched vs. Competitor Claims
The volume and quality of clinical research supporting probiotic products varies dramatically across the market. Many products rely on general probiotic research or single preliminary studies to support marketing claims, while others lack any clinical validation for oral health applications.
| Research Parameter | BioGaia Prodentis | Leading Competitor A | Leading Competitor B | Generic Products |
|---|---|---|---|---|
| Total Clinical Studies | 60+ studies | 8 studies | 3 studies | 0-2 studies |
| Randomized Controlled Trials | 48 RCTs | 2 RCTs | 1 RCT | Rare |
| Total Participants | 2,355 participants | 240 participants | 80 participants | Variable |
| Publication Quality | Peer-reviewed journals | Mixed quality | Limited peer review | Often unpublished |
The extensive research portfolio supporting BioGaia Prodentis includes studies published in high-impact dental and medical journals, providing healthcare professionals with confidence in recommending these products to patients. This level of scientific validation is unmatched in the oral probiotic market.
Manufacturing Standards: GMP Certification and Quality Control
Manufacturing quality significantly impacts probiotic viability, potency, and safety. Products manufactured under Good Manufacturing Practice (GMP) standards undergo rigorous quality control testing to ensure consistent potency and purity throughout the product shelf life.
BioGaia Prodentis is manufactured in FDA-inspected facilities following pharmaceutical-grade GMP standards. Each production batch undergoes comprehensive testing including bacterial viability counts, contamination screening, and stability analysis. This rigorous quality control ensures that patients receive products containing the labeled bacterial counts in viable form.
Many generic probiotic products lack adequate quality control measures, resulting in significant variability in bacterial viability and potency. Independent testing has revealed that some products contain less than 10% of labeled bacterial counts, while others show contamination with potentially harmful microorganisms.
The stability testing protocols for BioGaia Prodentis ensure maintained potency throughout the product shelf life when stored according to manufacturer recommendations. This reliability is crucial for achieving consistent therapeutic outcomes in clinical practice.
Frequently Asked Questions
Order Your Discounted BioGaia Prodentis Bottle Now!